Regeneration of skin damage
Let's look at the main nuances of skin regeneration.
The mechanisms of wound healing and scar formation have been studied for a very long time. But even today there are many molecular nuances that are not fully understood. In practice, it is important for a dermatocosmetologist to understand the basics of skin structure renewal processes in order to carry out safe and effective procedures.
Olga Maslova , candidate of biological sciences, cell biologist
It is important to consider wound healing at a general physiological level, taking into account the systemic reactions of the body. Cell biologists are primarily interested in intercellular communications and the molecular cascades that ensure them. The questions are so complex that almost every scientific article ends with some variation of the phrase “further study required.”
There are several classifications of wound healing stages. Depending on the type of damage and other features, some stages may manifest themselves to varying degrees, but in general the following stages can be noted.
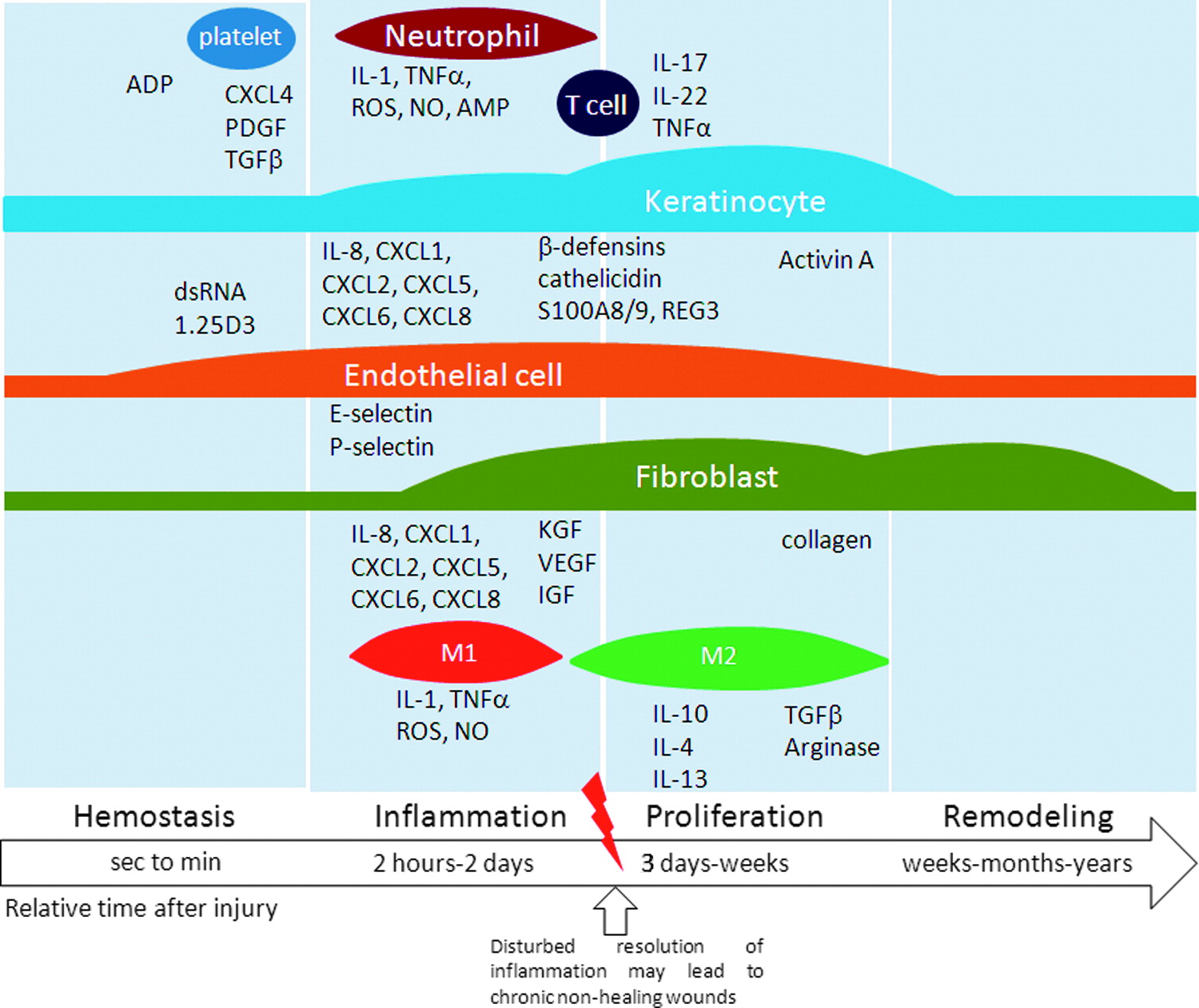
The very first and often very short (usually measured in minutes, as it takes from seconds to several hours) phase is hemostasis - that is, the blood clotting process that draws platelets and leukocytes into the wound. Separately, the process of blood coagulation and clot formation is described in detail.
Directly for wound healing, the release of a number of signaling molecules from platelet alpha granules is important, which can already be considered part of the next stage - inflammation , which will last from several hours to several days, and in some cases may last for a longer period. This phase is characterized by high activity of immune cells, mainly neutrophils, which fight infection and also release their signaling molecules that can coordinate the activities of other cells.
At the same stage, macrophages are included in the work, which, depending on the type, can perform different functions: macrophages M0 - are at rest, M1 - participate in this phase (pro-inflammatory), M2 - participate in the next phase of proliferation (anti-inflammatory or reparative).
Macrophages not only “scavenge” after neutrophils (phagocytosing debris and remnants of infectious agents), but also release many signaling molecules that involve other types of cells in the process. The inflammatory phase involves different immune cells, depending on the need and the properties of the damage.
The next phase is considered to be the proliferation phase, that is, the restoration of the number of cells. This is where the anti-inflammatory population of macrophages and the main players, fibroblasts, come into play. At this stage, it is important to remove all the “hysteria” of the immune system, since the body (if the previous phase has been successfully completed) receives a signal that “the enemy is defeated” and it is time to reduce the intensity of aggressive actions and slowly clean up the battlefield and mechanically build up the territory.
Fibroblast is one of the most mysterious cells in our body. There are many cells of this type, they are found in different places, but the main feature of a fibroblast in the process of damage healing is its dynamism and “kinship” with a mesenchymal multipotent cell. There are several classifications of fibroblast differentiation and different formulations for determining proximity to a mesenchymal multipotent cell, but roughly one can imagine a fibroblast as a certain functional state, which under some conditions ensures the synthesis of the extracellular matrix and the release of one group of signaling molecules, and under other conditions it “reformats” into a proliferative an active cell with a different set of secreted signaling molecules.
For wound healing, the process of “epithelial-mesenchymal transitions” is very important, which is characterized by the fact that the conditionally mobile mesenchymal phenotype allows the cell to move to the place of greatest need, and there to “anchor” and turn into an element of a stable epithelium, the cells of which are not able to move. Normally, such transitions occur only during the process of intrauterine development and wound healing. They are also an important part of the development of cancer, as they take part in the spread of tumor cells. In wound healing, fibroblast works both as a “builder” and as a “manager” - regulating the proliferation and functioning of other cell types.
At the recovery stage, in addition to fibroblasts, multipotent cells themselves are also involved in the process, however, it is not always possible to distinguish them under these conditions. Different functional states of fibroblasts, from close to early mesenchymal to myofibroblast, are characterized by different properties and tasks (sometimes opposite in effect). A lot of work is now devoted specifically to the interactions of fibroblasts with other types of cells. It turns out that fibroblast can “find an approach” to many cell types and, depending on the situation, is able to release different substances that modulate the work of “colleagues”. Depending on the severity of the damage, the proliferation phase can take from several days to several weeks and includes both restoration of the skin itself and deeper work involving the reconstruction of vascularization and innervation. Accordingly, different groups of cells will be involved in such cases.
At the recovery stage , stem cells of varying degrees of potency from multipotent to unipotent (precursor cells) and different embryonic origins play an important role, because it is necessary to restore the entire tissue structure layer by layer and paracrine “guide” all regenerative processes. It is known that skin stem cells are represented by derivatives of different germ layers: in the basal layer of the epidermis there are cells formed from the ectoderm, in the dermis - from the mesenchyme, in the hair follicles - from the neural crest, plus there is a separate population - the precursors of melanocytes. Each of these types performs its own tasks, restoring tissue and returning the microenvironment to a calm state. With extensive damage leading to a systemic reaction, stem cells often “come” to the lesion from neighboring layers or even large depots of multipotent cells. This happens due to a phenomenon called homing - the ability of a stem cell to move around on an emergency call. With the help of receptors on its surface, the cell picks up signals for help and “rushes” along the concentration gradient of the chemical signal to the place where it is needed most at the moment.
The next stage is remodeling , which can occur over a long period. At this stage, all structures created by fibroblasts “in haste” are replaced: collagens are replaced, the appearance of the wound site is put in order, and everything returns to the form as close as possible to the “pre-damage” period. The success of this phase depends on the degree of damage and the regenerative potential of the body.
At each stage, unfortunately, a failure can occur and then the body deals with pathological wound healing, which can be expressed in different ways. Sometimes fibroblasts can be “too careless” about the aesthetics of the process and go too far with collagen synthesis without tracking its characteristics - then, for example, scars appear. Sometimes all processes go wrong (this can be especially pronounced at the border between the phases of inflammation and proliferation) and healing is not completed, leading to chronic wounds and even ulcers.
Source: The Innate Immune System in Acute and Chronic Wounds 2015 DOI: 10.1089/wound.2014.0608
*Hemostasis – inflammation – proliferation – remodeling; From seconds to minutes --- 2 hours – 2 days --- 3 days – weeks --- weeks-months-years; Relative time since injury; Impaired resolution of inflammation can lead to chronic, non-healing wounds
In general, the effectiveness of wound healing can be influenced by many factors, including genetic characteristics, the condition and number of stem cells (of different types), localization of damage, different levels of expression of growth factors, cytokines, etc., age, the presence of diseases (especially diabetes ), the picture of the existence of the microbiome and infection in the body, circadian rhythm, the work of the catecholamine system, the balance of neurotransmitters, the phase of the cycle for women.
First published: Cosmetologist No. 1, 2019
Read also
- Next-generation lipofilling
- The Importance of Post-Procedure Care for the Outcome of Aesthetic Treatments
- Cosmeceuticals in action: skin restoration in the neck and décolleté area
- Intensive damaging procedures: how to shorten the rehabilitation period
- Skin regeneration: biology of the process and methods of its stimulation
- Stimulation of skin metabolism: possibilities of transmembrane protein
- Stimulated skin regeneration: how to minimize risks and achieve long-lasting results. Online conference
- Injection options for treating hypertrophic scars
- Pathogenetic features of hypertrophic scars