Skin restoration after tattooing: medical aspect in permanent makeup
What you need to know the master of permanent makeup

Permanent make-up is indispensable without damage to the skin, albeit minimal. The process of skin regeneration will go on as usual: phase by phase. Let's try to present each of them in detail.
Since during tattooing the drawing is applied not with a brush, but with a needle, then there is no way to do without damage to the skin, albeit minimal. And to see the result of permanent makeup in all its glory, you will have to wait a few days with patience. Meanwhile, the process of skin regeneration will go on as usual: phase by phase, stage by stage. Let's try to present each of them in detail.
phase of inflammation
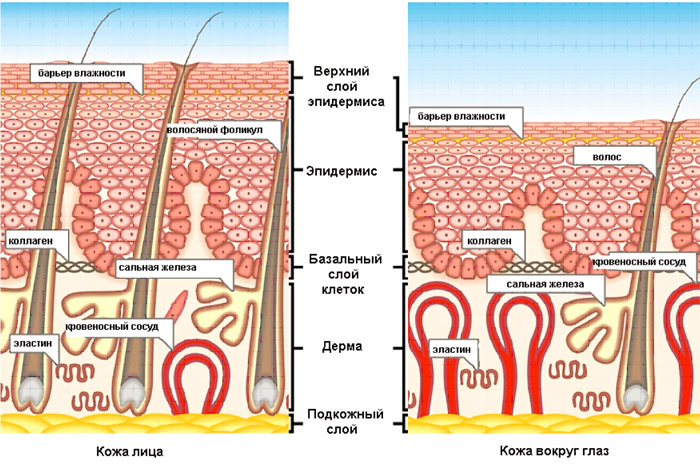
In this phase, the needle damages all the structural components of the skin - the epidermis, blood vessels located in the superficial vascular plexus of the dermis, cells and fibers of the connective tissue.
In response to damage, the skin responds with a universal local protective vascular-stromal reaction, or simply inflammation. Its signs are well known to all. This is redness, swelling and local fever, as well as pain that occurs due to injury to nerve endings.
The inflammatory reaction around the injury consists of several stages: first, there is vasodilation (a sharp expansion) of blood vessels and an increase in the volume of circulating blood, which means that intravascular pressure increases. This leads to thinning of the vascular walls, in which additional pores open.
Further, the process passes into the stage of exudation (literally - sweating): through the thinned wall and enlarged pores, the most liquid component of the blood begins to flow - plasma, which seeps into nearby tissues. As a result, interstitial pressure increases, which leads to edema. Following the blood plasma, approximately 2–4 hours after tattooing, leukocytes approach the damaged area. They create an infiltration leukocyte shaft around this zone. These cellular elements carry out phagocytosis of destroyed cells, gradually absorbing and "digesting" them. Thus, necrolysis (purification) occurs in the damaged tissue.
At the site of damage to the skin, blood and plasma (lymph) come to the surface and, drying up, form a crust, or scab. This crust protects the site of injury for the duration of the wound healing.

Phase of proliferation (reproduction)
This phase begins on day 2-3. Along the edges of the wound, increased cell division occurs, from which tubular formations are formed, having the appearance of a kidney at the end. They grow towards each other and, connecting with each other, form capillary vascular loops, which, in turn, begin to branch until they find an exit into a larger vessel. Thus, the circulatory system is restored in the damaged area, which begins to intensively supply the affected area with oxygen and nutrients, stimulating the healing and regeneration processes. Approximately on the 4th day, an increased migration of fibroblasts begins in the adjacent tissues, which form a granulation tissue that covers the wound. This thinnest layer of new cells serves as the basis for subsequent epithelialization of the wound surface. Fibroblasts are also involved in the synthesis of collagen fibers, which give strength and elasticity to the replenished tissue, as well as in the reproduction of proteoglycans, which form a jelly-like substance of the extracellular space. In the process of proliferation, the number of nucleoproteins, glycosaminoglycans, hyaluronic acid increases. There is a growing number of connective tissue cells (mast cells), which contain in their cytoplasm histamine and heparin, which regulate blood viscosity. Their number is maximally increased by 5-7 days.
Tissue regeneration can be stimulated using appropriate preparations (for example, Solcoseryl) or ointments containing ginseng, Chinese magnolia vine and other biologically active substances that promote tissue repair.
Phase of epithelialization
This phase begins immediately after the procedure and intensifies on days 3-4. Epithelialization is the growth of young skin that occurs simultaneously with the formation of connective tissue. In the dermis, epithelization completes the healing process. The cells of the basal layer of the epidermis begin to intensively divide and "creep" from the edges of the wound to its center, forming the basement membrane and, thereby, filling the defect formed in it. From the periphery to the center of the wound, a regenerated epithelium is advancing on the young connective tissue. This process will continue until the skin is completely restored. Cornification in new cells will be slow at first, but by the end of healing it may even become excessive. Upon completion of epithelialization, the granulation tissue gradually turns into connective tissue. After the rejection of the scab on the 3-5th day, the edges of the wound begin to peel off intensely, a large number of horny scales appear, then this process fades.
Clients are strongly advised not to remove the scab, even if it itchs and causes anxiety. It is also not necessary to soak the formed crust, since this can lead to its premature rejection, and then the tissues deprived of cover will be completely defenseless against infection. The healing of tissues under the crust goes in parallel with the fading process of inflammation, which usually ends on the 5-7th day.
Soon after tissue repair, the tattoo fades a little, because a small veil of collagen fibers forms around the pigment crystals that remain in the reticular and papillary layers of the skin. They braid literally every particle of the pigment, enclosing it in a thin capsule, which makes these crystals inaccessible to the immune system.
A favorable healing scenario has been described here. But if an infection has joined in the process, things can take a completely different turn. The resulting purulent inflammation will not only greatly slow down the closure of lesions with new skin, but a scar may form in its place. This process is called healing by secondary intention, or healing by suppuration. In this case, you should seek the advice of a dermatologist as soon as possible and in no case self-medicate.
It is also known that you should not do permanent makeup during a cold, and also if there are at least minor inflammatory processes on the skin (pustules, acne, herpes). In addition, it is undesirable for women to turn to permanent makeup during menstruation, since at this moment the pain syndrome usually increases, blood clotting decreases, and wound healing is slower.