Skin pH and its microflora: how are they connected?
The skin is the largest organ, with an area of up to two square meters in an adult. Let's figure out what skin acidity is, what the pH level should be and what to do if the acidity is disturbed.
Svetlana Tkachenko, Candidate of Medical Sciences, Associate Professor of the Department of Dermatology, Venereology and Medical Cosmetology, Kharkov National Medical University (Kharkov)
Close community
The surface of the skin is not sterile; it is a complex ecosystem of bacteria, fungi and viruses, which today is called the microbiome. Such a community can be symbiotic or parasitic regarding the physical and immune status of the host.
All normal human microflora is divided into resident (permanent, non-pathogenic), constituting up to 90% of microbes present in the body, facultative (temporary, opportunistic) - less than 9.5%, and transient (random, pathogenic) - up to 0.5%. About 20% of the total number of microorganisms lives in the oral cavity (more than 200 species), 18-20% in the skin, 15-16% in the pharynx, 2-4% in the urogenital tract in men and approximately 10% in the vaginal biotope among women. Most microorganisms (up to 40%) live in the gastrointestinal tract.
Despite the variability of external conditions, the skin maintains a stable microbiological ecosystem. The skin temperature is slightly lower than normal body temperature, its surface is slightly acidic and mostly dry, while most bacteria require a neutral pH, a temperature of 38 ° C and high humidity for optimal growth. Therefore, it is the physiology of the epidermis and the microenvironment it creates that dictate the microbial spectrum and population density. The acid mantle, mineral and hydration levels, the use of cleansers and cosmetic influences can influence the composition of human skin microflora, and this influence can be both positive and negative.
Lasting protection
Acidic pH creates conditions for resident microorganisms, which maintain the biological stability and cleanliness of the skin and provide its protection from pathogenic microorganisms. It is believed that perhaps the pH of the skin is just one way to protect itself from germs. The top layer of skin is very dry and tightly packed, making the first line of defense unfavorable for many bacteria. The salty secretion of the sweat glands makes the microenvironment hyperosmolar, and this is also unfavorable for bacteria. Beneficial flora grows better at an acidic pH, while pathogenic bacteria - Staphylococcus aureus - grow better at a neutral pH. One study found that an acidic skin surface pH (4.0–4.5) keeps resident bacteria attached to the skin, while an alkaline pH (8.9) increases the dispersion of bacteria throughout the skin. As is known, the antimicrobial function of the skin is sharply reduced in such dermatoses as atopic dermatitis and childhood eczema, and this is a direct consequence of its alkalization down to neutral values. A high density of bacteria is found in areas of the skin with higher humidity and a more alkaline pH: inguinal folds, anal area, submammary folds, armpits. Relatively dry and exposed areas of the skin have a lower pH and a lower density of microorganisms. For example, the inner surface of the forearms has a bacterial population of 102-103 cfu/cm2 (cfu - colony forming units), compared to 105 cfu/cm2, respectively, present in the armpit area. Artificial occlusion of the forearm leads to a significant change in skin pH, composition and density of bacterial strains. For example, in one study, skin pH was 4.38 before occlusion, and after 5 days of occlusion it increased to 7.05. Similarly, the number of bacteria per unit area before occlusion was 1.8 × 102 cfe/cm2 and increased significantly to 4.5 × 106 cfe/cm2 after 5 days of occlusion. Therefore, when carrying out occlusive procedures (wraps, wraps, bandages, latex and paraffin masks), the cosmetologist should remember the inevitable growth of microflora in the affected area and carry out preventive sanitation of the skin if this effect is undesirable.
Characteristic places of "settlement"
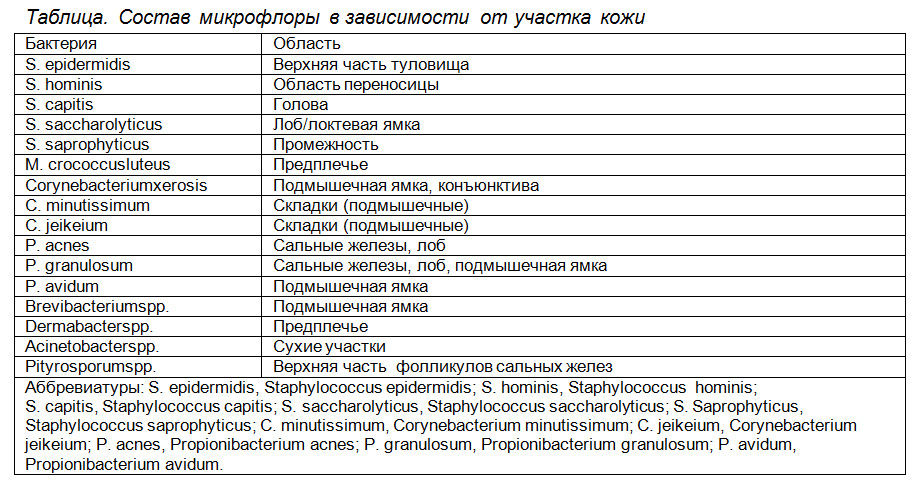
Resident bacterial strains isolated from normal skin include some staphylococci, micrococci, corynebacteria, brevibacteria, propionibacteria, and acinetobacteria. Transient pathogenic colonizers include Staphylococcus aureus, Streptococcus pyogenes, Escherichia coli, and Pseudomonas aeruginosa, which is considered an indicator of fecal contamination. The yeast is rare on the surface of the skin, but the lipophilic fungus oval pityrosporum is occasionally found on the scalp.
Recent studies using molecular techniques have provided a more complete understanding of the skin microbiome. 182 strains of bacteria were isolated and identified from the skin of the human forearm, of which 8% were unknown and had never been described before. In addition, some gender characteristics of the skin microflora were identified. Half of the bacteria identified in the samples turned out to be represented by the genus Propionibacteria, Corynebacteria, Staphylococcus, Streptococcus, which are usually considered as normal flora of human skin. Some bacteria were found only in men: Propionibacterium granulosum, Corynebacterium singulare, Corynebacterium appendixes.
This microflora is considered normal and its detection during cultural examination does not require sanitation and the prescription of antibiotics for treatment.
The skin of a newborn is sterile and begins to be populated by microflora shortly after birth. At the same time, the skin surface allows colonization and growth of only those bacteria that protect the host from pathogenic microorganisms directly or indirectly. Colonizing bacteria can produce antibiotics (bacteriocins), toxic metabolites, preemptively join competing bacteria, inducing a low redox potential, and deplete nutrient resources. Normal flora acts as a barrier and serves to prevent invasion and growth of pathogenic bacteria. Healthy growth and retention of resident flora effectively prevents colonization by transient pathogenic bacteria (E. coli, Pseudomonas, S. aureus, C. albicans). However, skin infection does occur, and in some people it is persistent and long-lasting.